The Centene Prior Authorization Form PDF is a crucial document used by healthcare providers to request pre-approval for specific treatments or medications. It streamlines the authorization process, ensuring efficient patient care and adherence to insurance policies. This form is essential for healthcare providers and patients to navigate the complexities of prior authorization requirements effectively.
1.1 Overview of Centene and Prior Authorization
Centene is a leading healthcare enterprise that provides high-quality medical services and insurance solutions. Prior authorization is a critical process requiring healthcare providers to obtain approval before prescribing certain treatments or medications. Centene implements this process to ensure safe, cost-effective, and medically necessary care. By streamlining prior authorization, Centene aims to enhance patient outcomes while managing healthcare costs effectively. This process is essential for maintaining quality and accessibility in healthcare services.
1.2 Importance of the Prior Authorization Form in Healthcare
The prior authorization form plays a vital role in healthcare by ensuring that treatments and medications are medically necessary and cost-effective. It helps prevent unnecessary prescriptions, reduces healthcare costs, and promotes safe patient care. For providers, the form streamlines communication with insurers, while patients benefit from access to approved treatments. By standardizing the approval process, the prior authorization form enhances efficiency and transparency in healthcare delivery, making it an essential tool for both providers and payers.
What is the Centene Prior Authorization Form?
The Centene Prior Authorization Form is a document used by healthcare providers to request pre-approval for specific treatments or medications, ensuring compliance with insurance policies.
2.1 Definition and Purpose of the Form
The Centene Prior Authorization Form is a standardized document used by healthcare providers to request pre-approval for specific medications or treatments. Its primary purpose is to ensure that prescribed therapies meet medical necessity and cost-effectiveness criteria set by Centene. By requiring this form, Centene aims to streamline the approval process, reduce unnecessary treatments, and promote evidence-based care. The form serves as a critical step in ensuring that patients receive appropriate and covered treatments while adhering to insurance policies and guidelines.
2.2 Key Sections of the Centene Prior Authorization Form
The Centene Prior Authorization Form includes essential sections such as patient demographics, prescriber information, and medication details. It requires the drug name, dosage, and frequency, along with the patient’s medical history. Additional sections include clinical rationale for the requested treatment and supporting documentation. A provider certification section ensures the request is medically necessary. These sections collectively facilitate a comprehensive review process, ensuring adherence to Centene’s guidelines and promoting appropriate patient care.
How to Obtain the Centene Prior Authorization Form PDF
- Download directly from Centene’s official website under the “Forms” section.
- Access the form via the CoverMyMeds platform for electronic prior authorization.
- Obtain it through healthcare providers or by contacting Centene’s customer support.
3.1 Downloading the Form from Centene’s Official Website
To download the Centene Prior Authorization Form PDF, visit Centene’s official website and navigate to the “Forms” section. Locate the “Prior Authorization” category and select the appropriate form for your needs. Ensure you choose the correct version based on your state or specific health plan. Once selected, click the download button to save the PDF to your device. Make sure to review the form for any specific instructions before completing it. This method provides quick and direct access to the necessary documentation.
3.2 Accessing the Form via CoverMyMeds Platform
CoverMyMeds is Centene’s preferred platform for electronic prior authorization (ePA) services. To access the Centene Prior Authorization Form PDF, visit the CoverMyMeds website and log in to your account. Navigate to the “Forms” section, where you can search for Centene-specific prior authorization forms. Select the appropriate form, download it, and fill it out electronically. This platform streamlines the process, allowing for faster submissions and reducing paperwork. It also provides real-time updates and tracking for pending authorizations, enhancing efficiency for healthcare providers and patients alike.
3.3 Obtaining the Form Through Healthcare Providers
Healthcare providers often have direct access to the Centene Prior Authorization Form PDF and can provide it to patients or their representatives. Patients can request the form during office visits or by contacting their provider’s administrative staff. Additionally, some providers may offer the form through their patient portals or via email. This method ensures personalized assistance and verification that the correct form is used for specific treatments. Providers may also guide patients on filling it out accurately, streamlining the prior authorization process and reducing delays in treatment approvals. This direct access is particularly beneficial for those with limited online access or preferring face-to-face interactions.
Filling Out the Centene Prior Authorization Form
Filling out the Centene Prior Authorization Form requires specific details like patient and provider information, medication specifics, and medical justification. CoverMyMeds simplifies the process.
4.1 Required Fields and Information
The Centene Prior Authorization Form requires specific details to ensure timely processing. Key fields include patient demographics, provider information, medication name, dosage, and frequency. Additional sections demand medical justification, diagnosis codes, and treatment duration. Accurate completion of these fields is essential to avoid delays. Proper documentation, such as medical records or test results, may also be necessary to support the request. Ensuring all required information is provided and legible is crucial for a smooth authorization process.
4.2 Documentation Needed for Submission
Documentation needed for submission includes medical records, test results, and medication history. These documents provide context for the treatment and support the prior authorization request. Including dosage details and treatment duration is also essential. Proper documentation ensures the request is processed efficiently and meets Centene’s requirements. Submitting complete and accurate information helps avoid delays and supports timely patient care. Ensuring all documents are legible and well-organized is crucial for a smooth review process.
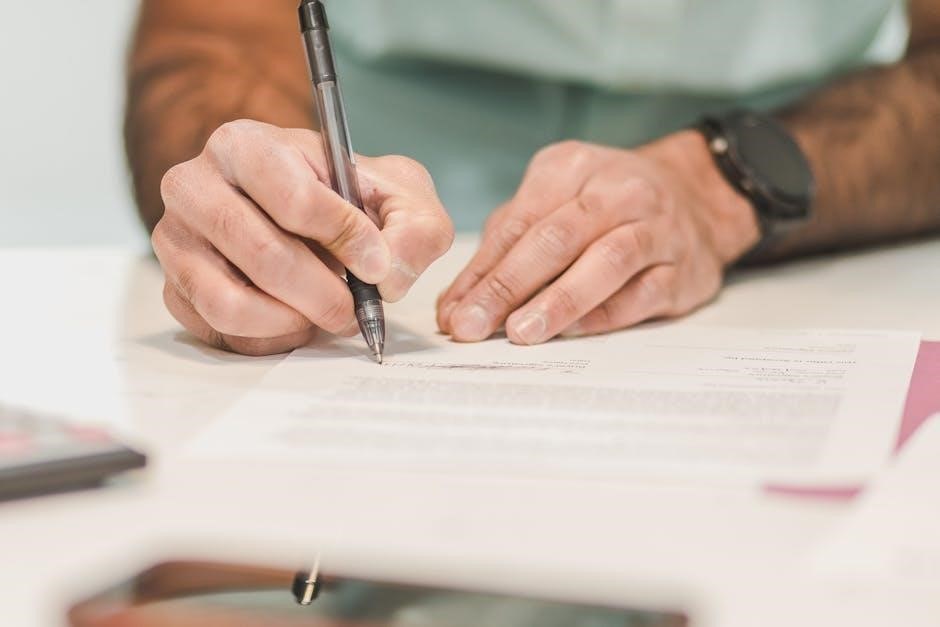
4.3 Step-by-Step Guide to Completing the Form
Download the Centene Prior Authorization Form PDF from their official website or via CoverMyMeds.
Fill in patient demographics, provider information, and drug details.
Specify dosage, frequency, and treatment duration.
Attach medical records, test results, and medication history.
Ensure all required fields are complete and accurate.
Obtain the prescribing physician’s signature.
Review the form for errors before submission.
Submit via fax, mail, or online portal.
Keep a copy for your records.

Submitting the Centene Prior Authorization Form
Submit the completed form via fax, online portal, or mail. Ensure all required fields are filled accurately to avoid delays in processing the request.
5.1 Fax Submission Guidelines
To submit the Centene Prior Authorization Form via fax, ensure all required fields are complete and legible. Use the designated fax number provided by Centene for prior authorizations. Attach any additional documentation as specified. Verify the fax number on the form or Centene’s official website to avoid errors. Keep a confirmation page for your records. Incomplete forms may delay processing. Ensure the fax is sent to the correct department to expedite the review process. Double-check all details before sending to prevent any discrepancies.
5.2 Online Submission Through Centene’s Portal
Submitting the Centene Prior Authorization Form online through Centene’s portal is a convenient and efficient method. Providers can create an account, upload the completed form, and submit it directly. Ensure all fields are filled accurately and required documentation is attached. The portal allows real-time tracking of the submission status. Once submitted, a confirmation receipt is generated for records. This method reduces processing time and ensures faster reviews. It is also environmentally friendly and minimizes the risk of lost documents. Always verify the portal’s requirements before submission for a smooth experience.
5.3 Mailing the Completed Form
Mailing the Centene Prior Authorization Form is a reliable method for submission. Ensure the form is fully completed and signed before mailing. Include all required documentation, such as medical records or prescriptions. Use a trackable shipping method, like certified mail, to confirm delivery. Address the envelope to Centene’s designated prior authorization mailing address, which can be found on their official website or the form itself. Allow sufficient time for processing, as mail submissions may take longer than electronic methods. Verify the address to avoid delays and ensure the request is processed promptly.

Checking the Status of Prior Authorization
Centene offers multiple methods to check the status of prior authorization requests, including online portals and direct contact with customer service. Use reference numbers for quick access.
6.1 Online Portal for Status Updates
Centene provides an online portal for convenient tracking of prior authorization requests. Members and providers can log in to check the status using reference numbers or patient details. The portal offers real-time updates, reducing wait times and enhancing transparency. Additionally, users can access historical requests and review decisions instantly. This digital tool streamlines communication and ensures efficient monitoring of authorization processes.
6.2 Contacting Centene Customer Service
For assistance with prior authorization, Centene offers dedicated customer service support. Members and providers can contact Centene via phone or fax to inquire about the status of requests or seek guidance. The toll-free number and specific fax lines for prior authorization are provided on their official website. Additionally, Centene’s customer service team is available to address questions, provide forms, and offer clarification on requirements. This support ensures timely resolution of issues and helps navigate the authorization process efficiently.

Common Mistakes to Avoid When Using the Form
Avoid incomplete or missing information, incorrect entries, and delayed submissions. Ensure all required fields and documentation are included to prevent processing issues and delays in approval.
7.1 Incomplete or Missing Information
Incomplete or missing information is a common mistake that can delay the processing of prior authorization requests. Ensure all required fields, such as patient demographics, drug details, and medical justification, are fully completed. Missing information, like dosage instructions or diagnosis codes, can lead to rejection or additional requests for clarification. Providers should double-check the form for accuracy and completeness before submission to avoid unnecessary delays in patient care. Attention to detail is crucial to ensure timely approval and uninterrupted treatment for patients.
7.2 Incorrect or Illegible Entries
Incorrect or illegible entries on the Centene Prior Authorization Form can lead to processing delays or rejection. Ensure all information, such as drug names, dosages, and patient IDs, is accurate and clearly written. Illegible handwriting or typographical errors can make the form unreadable, requiring resubmission. Double-check all entries for correctness and clarity before submitting. Using digital tools or electronic platforms, like CoverMyMeds, can help reduce errors and improve readability, ensuring smoother processing of prior authorization requests.
7.3 Delayed Submission and Its Implications
Delayed submission of the Centene Prior Authorization Form can result in treatment delays, impacting patient care. Timely submission ensures pre-approval processes are completed without interrupting therapy. Providers should prioritize submitting forms well before treatment starts. Late submissions may lead to denied requests or retroactive approvals, causing financial and operational challenges. Using electronic platforms like CoverMyMeds can expedite the process, reducing delays and ensuring continuity of care. Prompt action is essential to avoid negative outcomes for patients and administrative burdens for healthcare providers.
The Centene Prior Authorization Form PDF is essential for streamlining healthcare processes, ensuring timely approvals, and improving patient outcomes. Accurate and prompt submissions are crucial for efficient care delivery.
8.1 Summary of Key Points
The Centene Prior Authorization Form PDF is a vital tool for healthcare providers to request pre-approval for treatments or medications. It ensures compliance with insurance policies and streamlined care delivery. Centene has updated its system to expedite pre-approval decisions, benefiting both providers and patients. The form is accessible via Centene’s website, CoverMyMeds, or through healthcare providers. Accurate and timely submissions are crucial for efficient processing. Understanding and adhering to the form’s requirements helps avoid delays and ensures patients receive necessary treatments promptly. Proper documentation and compliance with guidelines are essential for successful submissions. Always refer to Centene’s official resources for the most updated information and instructions.
8.2 Final Tips for Efficient Use of the Centene Prior Authorization Form
For efficient use of the Centene Prior Authorization Form PDF, ensure all required fields are completed accurately. Double-check for missing or incorrect information before submission. Utilize electronic submission options like CoverMyMeds for faster processing. Always verify the form’s version and submit well in advance of treatment to avoid delays. Keep a copy of the submitted form for your records and follow up on the status through Centene’s portal or customer service. Stay informed about any updates to Centene’s policies or procedures to ensure compliance.